Connect With Us
Blog

High Heels Can Be Harmful
 Most little girls can’t wait for the day that they are able to wear high-heeled shoes. And while high heels often look attractive, down the road, they can eventually cause painful foot conditions. Aside from the obvious possibilities of falling or spraining an ankle, wearing high heels for extended periods of time can also lead to lower back and knee pain. If 5-inch heels are causing a problem, rather than switching to flats, a middle-of-the-road approach is suggested. Flat shoes can cause the Achilles tendon to become inflamed, and this may hurt the back of the heel. Wearing lower heels somewhere between 1 and 2 inches can help alleviate symptoms as well as a wider toe box. If your feet hurt, whether you wear high heels or not, it is a good idea to consult a podiatrist for an evaluation and treatment plan.
Most little girls can’t wait for the day that they are able to wear high-heeled shoes. And while high heels often look attractive, down the road, they can eventually cause painful foot conditions. Aside from the obvious possibilities of falling or spraining an ankle, wearing high heels for extended periods of time can also lead to lower back and knee pain. If 5-inch heels are causing a problem, rather than switching to flats, a middle-of-the-road approach is suggested. Flat shoes can cause the Achilles tendon to become inflamed, and this may hurt the back of the heel. Wearing lower heels somewhere between 1 and 2 inches can help alleviate symptoms as well as a wider toe box. If your feet hurt, whether you wear high heels or not, it is a good idea to consult a podiatrist for an evaluation and treatment plan.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact Kevin Powers, DPM from The Center for Lower Extremity Nerve Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact our offices located in Indianapolis and Bloomington, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Effect of High Heels on the Feet
High heels are uncomfortable, but many women sacrifice comfort to be stylish. There are many problems that stem from wearing high heels, however these issues can be avoided by wearing proper shoes.
Heels are bad because they push your weight forward toward the fall of the foot. The higher the heel is, the more weight and pressure get shifted. This process causes the back to hyperextend backwards to counterbalance which may cause pain in the leg, hip, and back. Consequently, major posture problems may occur, and these issues may eventually become permanent.
Wearing high heels is one of the leading cause of ingrown toenails. Heels create a great deal of pressure on the big toenails which disrupts proper toenail growth. This may eventually lead to the big toenail growing into the skin. Another common problem that stems from high heels is bunions. If bunions go untreated, they can cause serious scar tissue to form along with severe pain.
However, there are ways to minimize the harmful risks associated with wearing heels. You should try to massage and stretch your legs and feet after wearing heels for an extended time. Stretching helps prevent the Achilles tendons and calf muscles from becoming too tight. A good substitute for heels are platforms which provide a better surface area to evenly distribute the body’s weight.
If you are experiencing any painful foot conditions from wearing high heels, you should consult with your podiatrist right away.
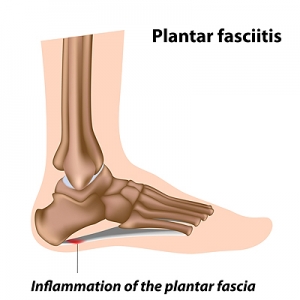
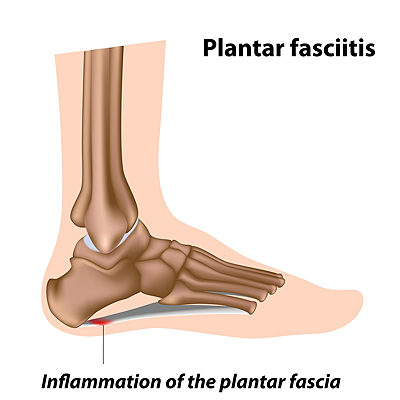
Why Do I Have Plantar Fasciitis?
Plantar fasciitis, the inflammation of the ligament that runs along the bottom of the foot and connects the toes to the heel bone, is a common cause of heel pain. When the plantar fascia is injured through repetitive strain, excessive exercise, prolonged standing, wearing uncomfortable shoes, or obesity, it may lead to stabbing heel pain that is typically at its worst when taking the first few steps after a long rest. Other possible causes of plantar fasciitis include structural abnormalities in the foot, such as having flat feet, high arches, overpronation, or leg length differences. Foot changes associated with aging or pregnancy may also be to blame in some cases. If you are suffering from heel pain, don’t hesitate to schedule an appointment with a podiatrist near you.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Kevin Powers, DPM from The Center for Lower Extremity Nerve Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Indianapolis and Bloomington, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
What Is the Tarsal Tunnel and Why Is It Causing Me Pain?
The tarsal tunnel is a narrow passageway on the inside of the ankle that is made of a thick band of fibrous tissue (flexor retinaculum) and ankle bones. Veins, arteries, muscles, tendons, and the tibial nerve pass through the tarsal tunnel. Certain conditions such as a ganglion cyst, nerve sheath tumors, fibrosis, and even injuries can tighten the already-narrow space within the tunnel and compress the tibial nerve. This can cause burning pain or tingling (paresthesias) along the tibial nerve, the inside of the ankle, or bottom (plantar) part of the foot. If you are experiencing this type of discomfort, contact a podiatrist. They will perform a physical examination and may suggest that an MRI be performed to visualize lesions that may be present within the tunnel. Both conservative and surgical treatments will be considered depending on the cause and severity of the condition and will focus on reducing pressure on the nerve and relieving pain.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Kevin Powers, DPM of The Center for Lower Extremity Nerve Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our offices located in Indianapolis and Bloomington, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which the tibial nerve, located in the tarsal tunnel in the foot, is compressed. The tibial nerve can become compressed from injury, such as an ankle sprain, flat feet, and lesions. Arthritis, diabetes, and varicose veins can also cause swelling and thus result in nerve compression.
Symptoms of tarsal tunnel syndrome include several different sensations in the sole of the foot, inside the ankle, and around the tibial nerve. These sensations include shooting pains, numbness or reduced sensation, pins and needles, burning, and tingling. Symptoms tend to worsen with greater activity to the area. In rare and severe occasions, this can change the muscles in the foot.
If you suspect you have tarsal tunnel syndrome, you should consult with your podiatrist. He or she will examine your medical history to see if you have a history of diabetes, arthritis, or flat feet. They will also check to see if you have suffered an injury to the area recently. An electrical test will be conducted to check if the nerve has been damaged. A simpler Tinel’s Test might also be used. This includes simply tapping the nerve to create a sensation. An MRI scan of the area may also be used.
Treatments vary greatly for tarsal tunnel syndrome. Treatments include both nonsurgical and surgical options depending upon the severity of the condition. Nonsurgical options include anti-inflammatory medication and steroid injections to the area. Orthotics, such as a splint or brace that immobilizes the foot, is another noninvasive option. For those with flat feet, custom shoes can be made to offer better foot support. Surgical options include a tunnel tarsal release, in which an incision is made behind the ankle down to the arch of the foot. This releases the ligament and relieves pressure off the nerve. Some doctors use a more minimally invasive surgery, where smaller incisions are made in the ankle and the ligament is stretched out.
If you are suffering from painful sensations in your foot, see a podiatrist who can determine if you are experiencing tarsal tunnel syndrome. Tarsal tunnel syndrome that is left unchecked can cause permanent nerve damage to the foot.
What Do Orthotics Do?
 Shoe inserts that are designed to relieve pain caused by various foot conditions are known as orthotics. Common foot conditions treated by orthotics may include corns and calluses, tendonitis, bunions, heel pain, and stress fractures. Orthotics can also help non-foot related issues such as correcting posture and alignment. Orthotics come in a variety of types, including custom made ones, cushioned ones that absorb shock, and pressure relieving orthotics that distribute body weight across the sole of the foot. A podiatrist will consider many factors when prescribing orthotics, which include any existing foot conditions, the structure of the foot, biomechanics, and the patient’s lifestyle. If you believe that orthotics are right for you, a podiatrist will be able to help point you in the right direction.
Shoe inserts that are designed to relieve pain caused by various foot conditions are known as orthotics. Common foot conditions treated by orthotics may include corns and calluses, tendonitis, bunions, heel pain, and stress fractures. Orthotics can also help non-foot related issues such as correcting posture and alignment. Orthotics come in a variety of types, including custom made ones, cushioned ones that absorb shock, and pressure relieving orthotics that distribute body weight across the sole of the foot. A podiatrist will consider many factors when prescribing orthotics, which include any existing foot conditions, the structure of the foot, biomechanics, and the patient’s lifestyle. If you believe that orthotics are right for you, a podiatrist will be able to help point you in the right direction.
If you are having discomfort in your feet and would like to try orthotics, contact Kevin Powers, DPM from The Center for Lower Extremity Nerve Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our offices located in Indianapolis and Bloomington, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
Wounds That Don't Heal Need to Be Checked
The Importance of Foot Care For Diabetics
 Neuropathy, a form of nerve damage, is known for causing a loss of feeling in the feet, and roughly half of all diabetic patients have some type of neuropathy. Because of this lack of feeling, many small problems with the feet may not be noticed and thus lead to the development of serious issues. To help avoid missing the small issues that can occur with the feet, there are some daily things that diabetic patients can do. Daily checks for cuts and wounds, regularly washing the feet, wearing shoes that fit right, and avoiding going barefoot are a few of the things that can be done to help care for the feet once they have lost some feeling. Along with regular checkups, diabetic patients should consult with a podiatrist if they notice a loss of sensation in the feet, a change in shape or color to the feet, or loss of hair on the feet.
Neuropathy, a form of nerve damage, is known for causing a loss of feeling in the feet, and roughly half of all diabetic patients have some type of neuropathy. Because of this lack of feeling, many small problems with the feet may not be noticed and thus lead to the development of serious issues. To help avoid missing the small issues that can occur with the feet, there are some daily things that diabetic patients can do. Daily checks for cuts and wounds, regularly washing the feet, wearing shoes that fit right, and avoiding going barefoot are a few of the things that can be done to help care for the feet once they have lost some feeling. Along with regular checkups, diabetic patients should consult with a podiatrist if they notice a loss of sensation in the feet, a change in shape or color to the feet, or loss of hair on the feet.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Kevin Powers, DPM from The Center for Lower Extremity Nerve Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Indianapolis and Bloomington, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.