Connect With Us
Blog

Obesity and the Feet
Obesity is a common problem in American society. Approximately one third of the U.S. population is obese. Obesity is defined as a body mass index greater than 30. Obesity has the power to affect different aspects of the body, and one of the most common problems it causes is foot pain. There have been many studies that found a connection between an increased BMI and foot problems. A simple activity such as walking up a flight of stairs can increase pressure on the ankle by four to six times.
Being overweight causes the body to compensate for the extra weight by changing the way it moves. Consequently, people who struggle with obesity commonly have arch problems in their feet. Obesity causes the arch to break by stretching the ligaments and tendons that hold the bones in the foot together. When the arch lowers, the foot may eventually fall flat. Collapsed foot arches fail to provide adequate shock absorption which eventually leads to foot pain. Other conditions that may be caused by flat feet are pronation, plantar fasciitis, weak ankles, and shin splints.
Foot problems that are caused by obesity may be treated by wearing proper footwear. Proper shoes will allow your feet to have better circulation around the arch and ankle. Additionally, those with obesity often discover that typical heel pain remedies are not effective for them. They will find that their plantar fascia is easily injured, and it is often inflamed. The best way to treat this problem is to implement lifestyle changes. A few good ways to improve your diet are to reduce calories, fill up on fruits and veggies, and to limit sugars.
Custom foot orthotics can prevent foot problems if you’re carrying excess weight or are trying to lose weight. The purpose of orthotics is to provide shock absorption to decrease the amount of stress on the joints to prevent arthritis.
High Heels and Morton’s Neuroma
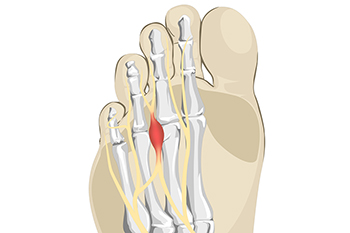
The pain that is felt from the foot condition that is known as Morton’s neuroma cannot be ignored. It is an ailment that affects the nerve that is found between the third and fourth toes, and can happen from frequently wearing high heels. These types of shoes often lack adequate room in the toe area, limiting the room for them to move freely in. This may ultimately lead to irritation and inflammation of the nerves, often causing pain and discomfort. The tissue surrounding the nerve can become thick, and patients may feel a sharp or burning pain. Additionally, people who have this type of pain may liken the sensation to walking on a marble, and often look for relief. This can be found when appropriate shoes are worn, and it is beneficial to frequently rest the affected foot. Maintaining a healthy weight may help to take the stress off of the overall foot. If you believe that you may have this condition, it is strongly suggested that you consult with a podiatrist who can effectively diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Kevin Powers, DPM of The Center for Lower Extremity Nerve Surgery. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Indianapolis and Bloomington, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
A Ruptured Achilles Tendon

Achilles tendonitis is a condition that can occur due to tears in the tendon from overuse. A ruptured Achilles tendon is an injury that happens when a sudden strain overwhelms the Achilles tendon. With a rupture, one will feel sudden and intense pain as well as a possible popping noise. Furthermore, there can be burning, swelling, and stiffness in the area. Sometimes it is hard to distinguish whether the Achilles tendon is ruptured, or if the pain is a result of a pulled muscle. However, if the pain is intense and does not go away or if there is greater than average stiffness in the area it is likely a rupture. It may also be a rupture when one does not pass the Thompson test, where the soleus complex is manipulated. This kind of injury does not heal quickly. One needs to rest and participate in physical therapy for proper healing. Because many of these symptoms can overlap with other afflictions, it is a good idea to make an appointment with a podiatrist for a proper diagnosis and treatment plan.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Kevin Powers, DPM of The Center for Lower Extremity Nerve Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Indianapolis and Bloomington, IN . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Causes, Types, and Treatments of Achilles Tendon Injuries
Tendons are fibrous tissues that connect muscles with bone. The Achilles tendon is the largest tendon in the body. It connects the calf muscles at the back of the leg with the heel, and facilitates movements such as jumping, running, and walking.
Because the Achilles tendon is engaged so frequently and bears a great deal of pressure and stress throughout the day, it can become injured. Achilles tendon injuries cause the tissue to become irritated, inflamed, and swollen. Pain can come on gradually or be immediate, and will vary from mild to severe depending upon the injury. Where the pain occurs will vary as well, from just above the heel up through the back of the leg. There may also be stiffness in the tendon.
Achilles tendon injuries can often be caused by repetitive stress. They may also occur while running, playing tennis, gymnastics, football, basketball, dancing, soccer, baseball or other sports that require speeding up, slowing down, or pivoting quickly. Wearing high heels, falling from an elevation, stepping in a hole, having flat feet, bone spurs, tight leg muscles or tendons, wearing improper athletic shoes, exercising on uneven surfaces, or starting a new type of exercise can also cause Achilles tendon injuries.
The two most common Achilles tendon injuries are tendonitis and ruptures. Tendonitis causes painful inflammation and can occur in different parts of the tendon. Non-insertional Achilles tendonitis occurs when the fibers in middle of the tendon begin to break down, thicken, and swell. This condition typically affects younger, more active adults. Insertional Achilles tendonitis occurs where the tendon inserts into the heel bone. It is common for bone spurs to form with this type of injury. This condition can affect people of any age and level of activity.
Achilles tendon ruptures are a tear in the tendon. These breaks may be partial or complete. There may be an audible popping noise at the moment of injury and the pain will be sudden and severe.
An Achilles tendon injury can be diagnosed by your podiatrist after they examine you, check your range of motion, and possibly perform a calf squeeze test or review an X-ray or MRI. Depending on the type and severity of your injury, your podiatrist may treat your condition with rest/ice/compression/elevation (RICE), nonsteroidal anti-inflammatory medications, heel lifts, and stretching and strengthening exercises. If you have torn your Achilles tendon, treatment may include physical therapy, ultrasound, shockwave therapy, or possibly even surgery.
Wounds That Don't Heal Need to Be Checked
Foot Conditions May Develop From Poorly Fitting High Heels

High heels are a popular type of shoe to wear, despite the foot conditions that may develop. Blisters are a common ailment that many women get, and they can occur on the back of the heels, or the sides of the feet. This can happen if the shoe doesn’t fit correctly, and women may use methods such as putting cotton balls in the shoes, or bandages where blisters would develop. Wearing high heels that do not have enough room in the toe area may cause Morton’s neuroma to develop. This is defined as irritation and thickening of the nerve that lies between the third and fourth toes. It can cause severe pain and discomfort, and the pain may be temporarily alleviated when lower-heeled shoes are worn. Additionally, these types of shoes can put stress on the joints and bones, possibly leading to getting a stress fracture. Any type of foot pain that comes from wearing high heels is treated by a podiatrist, and it is suggested that you consult with this type of doctor who can offer relief tactics, and recommend shoes that are better for your feet.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact Kevin Powers, DPM from The Center for Lower Extremity Nerve Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact our offices located in Indianapolis and Bloomington, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Effect of High Heels on the Feet
For hundreds of years, women have been wearing various kinds of high heels for aesthetic reasons. Women who wear high heels appear to be taller and have longer and thinner legs, and the wearer’s gait and posture changes. Though high heels have had an association with femininity and have kept them popular over the years, there are definite health problems caused by wearing them too frequently.
The motion of the ankle joints is limited when heels are worn. The ankle joint is very important to the body when it comes to walking. Because of their location, these joints have a great deal of weight put on them. Thus, it is very important to keep them as healthy as possible. The Achilles tendon is the main tendon in the ankle. Wearing high heels too often, studies have shown, can cause the calf muscle and Achilles tendon to shorten and stiffen. This can cause problems when shoes without heels are worn.
By putting a great deal of pressure on the ball of the foot and by forcing the toes into a small toe box, high heels can cause or may worsen many foot problems. These include corns, hammertoe, bunions, Morton’s neuroma and plantar fasciitis.
Not only does wearing high heels regularly have negative effects on the feet, the rest of the body can suffer as well. The knees, one of the most important joints in the entire body, can be affected by wearing high heels. High heels can cause the knees to stay bent all the time. Also, it can cause them to bend slightly inward as well. Doctors believe that women can suffer from osteoarthritis later in life because of constantly walking like in high heels. By limiting the natural motion of the foot during walking, high heels also cause an increased in stress on the knees.
Similarly, high heels can cause the back to go out of alignment. If high heels are worn constantly, the spine’s ability to absorb shock can cause continued back pain. They can compress the vertebrae of the lower back, and can overuse the back muscles.
However, this is not to say that high heels can never be worn. If worn occasionally and not often, they will not cause serious problems. They should not be worn every day. It’s important to wear them modestly to avoid the long-term physical health problems of the feet, knees, ankles, and back mentioned above.
Plantar Fasciitis Is a Common Foot Condition That Needs Podiatric Attention

The majority of plantar fasciitis symptoms will worsen without medical treatment. This condition is the inflammation of the plantar fascia, and it is considered to be one of the most common causes of heel pain. This is the portion of tissue that is located on the sole of the foot and connects the heels to the toes. The plantar fascia is responsible for shock absorption in addition to supporting the arch and the bottom of the foot. This condition can happen when the plantar fascia is stretched beyond its normal range, and it can happen from wearing shoes that do not fit correctly. Additionally, it is common among people who frequently run long distances, run on uneven surfaces, or stand for the majority of the day. The symptoms that many people experience with this condition can include severe pain and tenderness, swelling, and it can be difficult to walk. This may be worse in the morning upon arising, or after sitting for long periods of time. Plantar fasciitis generally gets worse before medical attention is sought. If you are afflicted with this condition, please consult with a podiatrist who can properly treat this condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Kevin Powers, DPM from The Center for Lower Extremity Nerve Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Indianapolis and Bloomington, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.