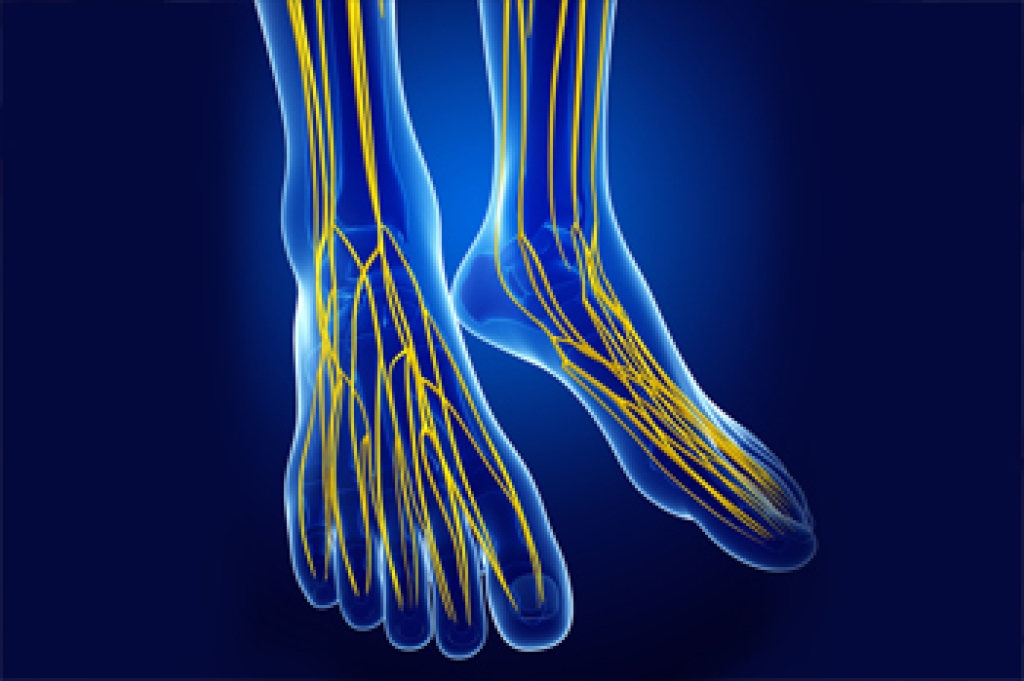
Heel pain is a very common occurrence. It is usually felt under the heel or at the back of the heel. When pain and inflammation is located on the bottom of the heel toward the front of the foot, plantar fasciitis is typically the cause. Plantar fasciitis is a painful inflammation of the plantar fascia tissue, which runs along the bottom of the foot and connects the heel with the toes. Other causes of heel pain on the bottom of the foot may be attributed to heel pad atrophy or heel spurs. If pain is felt at the back of the heel, Achilles tendonitis is often at the root of the cause. This condition occurs when the Achilles tendon, which attaches to the back of the heel bone, becomes damaged or torn over time, causing pain and swelling. Other possible causes include bursitis, Sever’s disease, and heel bumps. Pain from a heel stress fracture can occur anywhere on the heel, and tarsal tunnel syndrome can cause heel pain underneath the ankle bone. Heel pain can also be caused by neurological issues, infections and arthritis. Unless you suffer an acute injury, heel pain typically starts out mild, but can become severe. If you are experiencing any type of heel pain, don’t hesitate to contact a podiatrist to find out the cause and take measures to keep it from worsening or becoming chronic or debilitating.
Many people suffer from bouts of heel pain. For more information, contact Kevin Powers, DPM of The Center for Lower Extremity Nerve Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions, please feel free to contact our offices located in Indianapolis and Bloomington, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.